
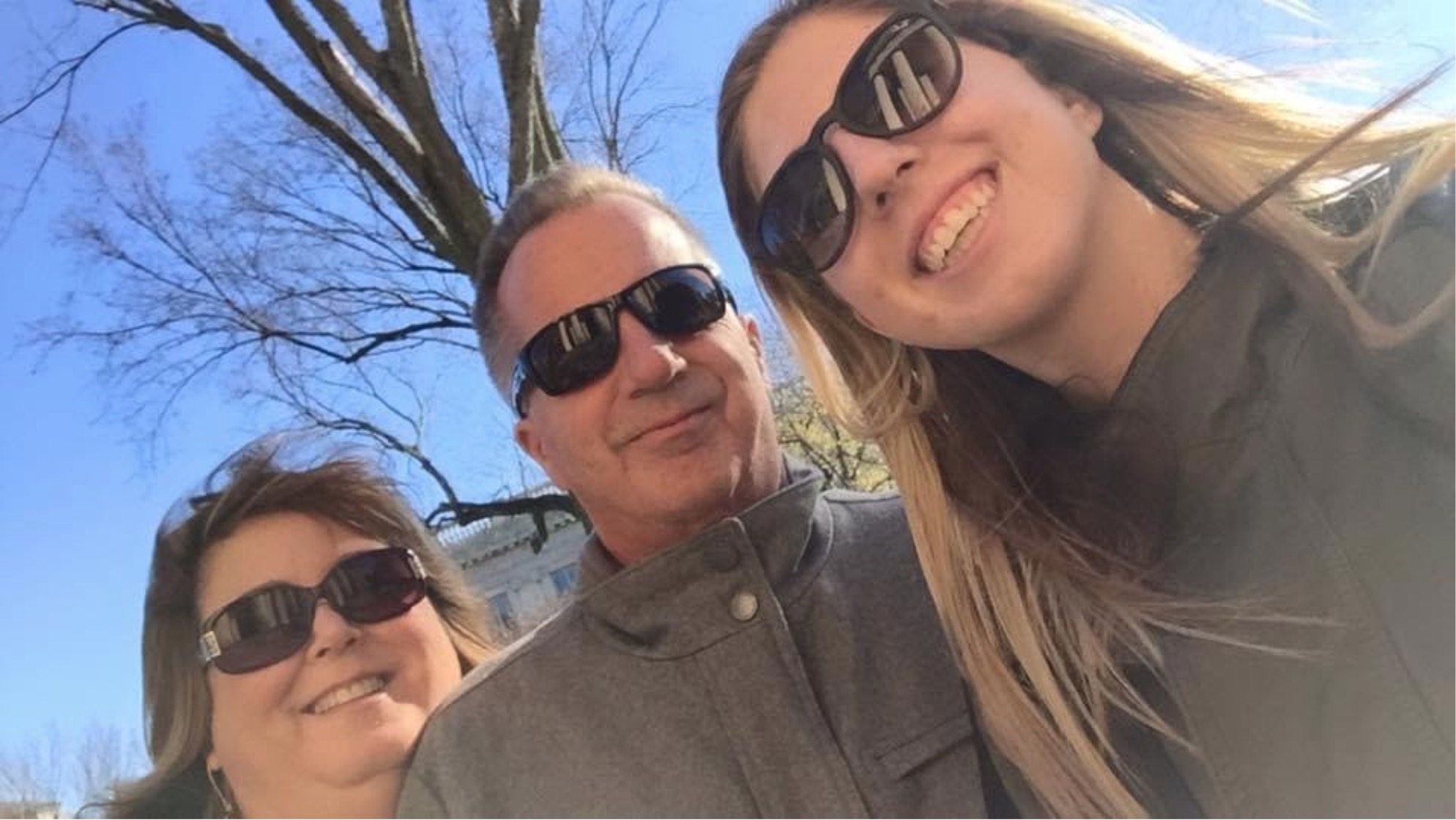
It wasn’t until last November, nearly four years after the death of her husband, that Jodie Quinn decided to publicly disclose how he died.
Even without being told, her daughter Shannon had known for years. At her father's funeral, anger burned inside of her when friends who had given him opioids showed up to pay their respects.
Although mother and daughter never discussed it at the time, or shared their feelings with the other mourners, Jodie was feeling a similar rage, amplified when one of the men who had fueled Michael’s drug addiction stood up to give a eulogy. To Jodie, he sounded as if he had known her husband his whole life, and he hadn’t.
“I try not to let the drugs be the thing that people remember about him, because he wasn’t just that,” Jodie now says, reflecting on her husband, Michael. “If that’s what you tell people, that’s all everybody says: ‘Oh, he died of an overdose.’”
Michael Quinn, of Wayne, New Jersey, died on February 8, 2018. He was 58 years old. After years of prescription opioid abuse, an overdose on cocaine precipitated the cardiac arrest that killed him.
Ever since she found him on their bed, not breathing, his wife has told people he died from a heart attack, choosing to omit any mention of the pills and other controlled substances that he had struggled with for several years.
A kind man with light blue eyes and a passion for cooking, Michael was 28 when he met Jodie, who was working as a receptionist for the same information technology company where he was employed. At the time she suffered from gout in her knees, and she remembers how when they moved in together, Michael would pick her up and carry her around the house. A few months later, when she spent weeks in a hospital recovering from kidney surgery, he would drive her mother to the hospital in New York, then back to New Jersey.
Jodie and their daughter, Shannon, meant everything to Michael. Whenever they went shopping—and he loved shopping—he would make them laugh by trying on the most absurd masks and hats he could find in the store. With his showman’s personality, his dream was to be a radio DJ. In college, he was the DJ for Susquehanna University’s radio station in Central Pennsylvania.
For his entire adult life, Michael traveled New York and New Jersey bringing software to new clients as an IT company’s outside salesman. As he drove the miles of freeway for work, he’d blast tunes by the band “Yes” on his car stereo.
But 30 years in a car traveling client to client took its toll. Over time, Michael developed bulging discs in his neck and back. As he gripped the steering wheel, the discs would pinch nerves in his back; severe pain would course up his spine.
At his doctor’s office in New Jersey, around 2009, he was prescribed his first bottle of Oxycontin. The opioids worked so well that Michael suggested that his wife take them for her own neck pain, which she did for a short time. But after seeing her husband become dependent, she switched over to less addictive medications and later stopped taking painkillers altogether.
Addiction runs in Michael’s family. Drinking bordered on alcoholism for his father and mother. Michael was always a frequent drinker and occasional pot smoker, but after his doctor started prescribing opioids, a pill accompanied his nightly glasses of wine. In 2016, when the IT company he worked for restructured and he was laid off from his job, he became depressed. Shannon and Jodie believe opioids and other drugs became a coping method, his way to dispel both physical and emotional pain.
As his drinking and drug use intensified, he sought out xanax and cocaine in addition to opioids.
Xanax, the top-prescribed antidepressant in the United States, gives feelings of stress relief. But more than 100,000 emergency room visits due to xanax misuse, often mixed with opioids, occur every year in the US, according to Medical News Today.
In the last two years of his life, opioids became an obsession for Michael. He would get together with a group of guys at the town bar and they would swap pills, tiding over those who hadn’t received a prescription that week. On the days he didn’t have opioids, he would be miserable, glued to the couch and refusing to leave the house.
As a high school student, Shannon Quinn saw her father take pills from an orange bottle multiple times a day. But it was only when she read the label and Googled the word “oxycodone,” that she realized that he had a serious addiction problem.
At the time, her cousin John, who was two years younger than her, was struggling with heroin addiction, which eventually led to his fatal overdose from fentanyl in 2016.
John lived five minutes down the street from her family and was like a brother to Shannon throughout her childhood. After John lost his dad to liver cancer at a young age, his coping mechanism became alcohol and drugs. At family dinners, Shannon would see track marks from heroin injection on his arm.
Together, Shannon and her mother struggled to get John to stay in treatment programs and stop using, but he didn’t want to, once choosing prison over rehab.
Her family members’ addictions weighed on Shannon as she went off to the University of Rhode Island for college. But it wasn’t until her junior year, when her cousin was having success in a rehab program, that she felt comfortable talking about it. She needed to share what she was witnessing, the heartbreak that comes from witnessing people you love abusing drugs.
Looking back now, Shannon says, “I definitely didn’t talk about it because of the stigma that relates to ‘oh, your cousin is a drug addict’ or ‘oh, your dad is abusing opioids.’ It was a very hard topic to talk about with my friends, so I kind of kept it to myself.”

By sharing her story, Shannon has found her support network expanded. She realized that many people she became friends with over the years had also had family members battle some kind of addiction or pass away from an overdose.
Shannon says she would have felt far less alone throughout high school and college if she had heard stories like hers. Today, she feels that sharing her experience is helping her process her grief and frustration. She wishes her mom would open up more.
“For the last two years of his life, it was pretty apparent that the drugstore store was a higher priority than I was and she was,” she says of her father. “So it's kind of hard for me to not talk about it.”
But Jodie is still hesitant to talk about her late husband’s addiction. She still hasn’t told her husband’s family the true cause of his death. Only her best friend, her daughter and her therapist know explicitly. Even to them, admitting her husband died from an overdose hasn’t been easy.
“You kind of whisper it. You don’t say it out loud,” she says.
Jodie is not alone in her hesitancy. Many families who lose a loved one to substance use are uncomfortable talking about it. The stigma surrounding addiction affects not only the drug user, but people who are living with or related to them.
This year, four advanced journalism students at Brown University combed through over 1,000 obituaries of people under 50 who died “suddenly” or “unexpectedly” in Rhode Island between January 2013 and January 2020, but the words “addiction,” “opioids,” or “overdose” rarely popped up. A mere 10 obituaries mentioned overdose, usually in the form of asking for donations to addiction recovery programs.
Craig Carpenter, funeral director of Carpenter-Jenks Funeral Home and Crematory in West Warwick— a town where 56 people died of overdose deaths from 2014-2019—says that in recent years, families who have lost loved ones to opioids rarely mention the cause of death in obituaries. Carpenter points to the sheer trauma of these events as being the cause of this trend. He says that an overdose-related death makes grief even more complicated because of its suddenness.
“For some it may be they consciously make that decision to not say anything. For others, and I think for most families, in the few days after a sudden death they are simply trying to process the loss,” he says. During this time, Carpenter often sees families grapple with the questions of how could they have not known or what more could they have done to help.
At her husband’s funeral, Jodie wanted to see him before any of the other mourners arrived. When she looked into the casket, she was in shock, wondering how this could have possibly happened. Jodie describes going through periods of anger and guilt.
Though the shock has subsided, the guilt she felt lingers, three years later.
“After his death, I kept asking myself, ‘Could I have been stronger and forced him to go into rehab?’,” she says. “Had I stopped him, had I been stronger, maybe he would have still been here.”
The persistent guilt makes discussing Michael’s drug use all the more difficult for Jodie.
What she likes to remember is “the guy that, when I was sick, would pick me up and carry me to the bed or the couch. Or the guy that made me laugh… I try not to remember the other stuff, because when I do, then I go back to blaming myself.”
But thanks to her daughter, Jodie now sees a therapist regularly, which she finds helpful in coming to terms with the loss of her husband and the stigma she has felt in discussing his drug addiction with others.
Dr. Alan Wolfelt, a grief counselor from the Center for Loss and Life Transition in Fort Collins, Colorado describes people unable to fully grieve for their loved ones as “forgotten mourners” who experience “disenfranchised grief.” Disenfranchised grief is defined by the Family Health Psychiatric and Counseling Center as grief that is not openly acknowledged, socially accepted, or publicly mourned.
“This often results in inhibition around acknowledging the reality of the death, reluctance to discuss the cause of death, difficulty in getting support from family and friends and reluctance to seek counseling or attend support groups,” Wolfelt says.
He says that these four things result in a vicious cycle of maintaining the stigma around addiction, leaving the mourner feeling alone and isolated.
In Jodie Quinn’s case, she was embarrassed about her husband’s addiction but also tried to hide it from others because she wanted to protect his reputation in life and in death. “I tried to hide it as best as I could,” she says. “Even my anger or frustration about all of it, I would hide from everybody.”
Siana Wood started the Rhode Island chapter of Grief Recovery After Substance Passing (GRASP) in 2011 after her brother, David, died from an overdose on a combination of alcohol and opiates. She said she started the group simply to find people who had suffered similar losses. Few friends or co-workers consoled her after her brother’s death. Some even questioned her as to why she was so upset.
The group Wood put together used to meet monthly at Warwick’s Anchor Recovery Center. GRASP, which has chapters throughout the country, also runs a Facebook page for their members, who span the US and Canada, where people can post about their grief. Wood believes GRASP provides a crucial substitute for the community so often lost or absent when a loved one dies from an overdose.
“A lot of that grief is very stigmatized because addiction is so stigmatized,” Wood says. “In the GRASP community we say, ‘When you lose somebody to opioid addiction, nobody brings you a casserole.’”
Stigma thrives on anonymity, according to Wood, and destigmatizing addiction and overdose demands telling the stories of individuals who overdosed and the families mourning them. When she speaks about her brother at events, she describes the hidden nature of his opioid addiction.
“My brother was a young father. He had a four year old son when he died. He was making almost six figures, he was working, he was highly functional until he couldn't function anymore and passed away that night.”
Though GRASP’s Rhode Island chapter has since gone dormant, support for stigma reduction campaigns is growing across the state, according to Lily Rivera, Assistant Director of Project Weber/RENEW, which provides naloxone and recovery support to opioid users in Rhode Island.
With an agenda of targeting stigma, the Rhode Island Department of Health has sought to spur public conversation about drug use. In May of 2018, Governor Gina Raimondo issued an executive order for a statewide campaign to improve attitudes towards addiction and mental health. The Governor’s Opioid Task Force, the body charged with carrying out the campaign, wrote in their strategic plan that “a society dominated by negative attitudes on addiction remains one of the biggest, most intractable barriers to seeking substance use disorder treatment, or for delivering effective substance use disorder care.” Along with equipping the public to administer naloxone, the Task Force has promoted town hall and dinner table conversations about behavioral health and stigma.
Another way Governor Raimondo has worked to end stigma is by putting people in recovery in charge, according to Brandon Marshall, Associate Professor of Epidemiology at Brown University. Marshall is the scientific director of Prevent Overdose RI, Rhode Island’s drug overdose surveillance and information dashboard.
“For a long time [the Governor’s] senior policy advisor on overdoses and addiction himself was in recovery,” said Marshall. “She listens to people in recovery and not only that, but she puts them in charge. So that helps destigmatize the issue. Not a lot of other state governments have done this to the same degree.”
Shannon Quinn recently joined the Governor’s Opioid Task Force. The Task Force will place her as a mentor to someone with a family member suffering from an addiction, and she’ll educate them on using naloxone, branded as Narcan, which is the drug used to prevent opioid overdose deaths.
The death of her father and cousin have also motivated Shannon’s career. She now works at the CVS Health Corporate Office in Woonsocket, advising pharmacies as a member of the Pharmacy Professional Practice Team. In her role at CVS, she supports a number of initiatives aimed at helping reduce opioid misuse, including CVS’s prevention education programs, in-store drug disposal, and naloxone initiatives. She has been partnering with the URI College of Pharmacy’s Community First Responder program to run events that certify people to identify an overdose and give them a Narcan kit. Seeking to support her daughter, Jodie took the online training and went to her pharmacy in New Jersey to equip herself with Narcan.
Rhode Island actress Ana Bess Moyer Bell is also trying to combat stigma through public awareness. She founded the drama therapy program Creating Outreach About Addiction Support Together (COAAST) in 2014, after she lost multiple friends to opioid overdoses.
COAAST, based in South Kingstown, stages plays where the characters talk about opioid addiction and substance use. After the curtain falls, the actors hold back and forth dialogues with the audience.
“I’ve stood on the stage in auditoriums where one kid in front of 600 kids will get up and say ‘I was taken away from my parents because they used heroin,’ and then it will ignite all these other kids to get up in front of each other and say a similar story,” Moyer Bell says.
“A lot of times with moms, they can talk about their children’s death, but they can’t actually name the reason why because of the stigma. It gives them a space to name the reason.”
This fall, Shannon Quinn attended one of COAAST’s events, staged outdoors in Pawtucket. She was touched when everyone in the crowd called out the names of loved ones they had lost to drugs. Her boss and her boyfriend, who have louder voices than her, helped her shout “John,” “Michael.”
“There were probably about 50 people there, and so many names were spoken,” she recalls. “It really just shows that you’re not alone.”
Jodie, who still lives in New Jersey, says she now feels open to attending a similar event if one were to be staged in her area. Her perspective has shifted in recent weeks, while speaking with her daughter for this story. For the first time, they discussed the anger and grief that they had each faced separately, things they had buried inside them for over a decade.
Jodie believes these conversations will lead to a more open relationship between them. Mother and daughter had always felt able to call each other for support when they were sad, but now they might be able to help each other deal with a tucked-away part of their grief—the guilt, frustration and feeling of helplessness that they’ve both experienced watching two family members eaten up by addiction.
— with reporting from Ivy Scott